This post was most recently updated on October 14th, 2019
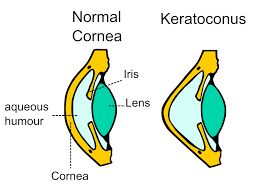
The cornea is part of the eye that is located on the front. It is clear, dome-shaped, and rests on top of both the iris and the pupil. A healthy cornea is strong and able to retain this cone shape while allowing sufficient light to proceed into the rest of the eye. The cornea is also responsible for helping the eye to focus. Approximately 65% to 75% of the eye’s ability to focus comes from a fully functional cornea. However, in some individuals, the cornea becomes weak and begins to thin. This causes abnormal bulging that changes the shape slowly over time to resemble a cone rather than a dome. When this happens, light is unable to transfer from the cornea to the retina properly, affecting vision.
In more severe cases, the bulging of the cornea can lead to tears which can result in scar tissue, causing permanent vision damage and the need for surgery. Unlike many other types of vision problems, keratoconus cannot be treated or resolved using glasses or standard contacts. The condition can continue to progress indefinitely if no treatments are put in place, but it has also been known to stop progressing without intervention. However, the disease can be treated with great success.
Causes of Keratoconus
More research is needed to fully understand what causes keratoconus. Certain correlations have been discovered, but it is still unclear whether these correlations are causes, symptoms, or both. It may be that an individual acquires keratoconus when several of these possible causes coincide.
Genetics behind Keratoconus
It is apparent that this thinning is, at least in part, a genetic disease. Although this condition only affects about 1 in 2,000 people, multiple family members will sometimes develop keratoconus. For this reason, children who have one or more parents with the condition are often encouraged to have their eyes checked often for abnormalities. Although the disease usually does not present itself until after puberty or in a person’s early 20s, it can be detected sooner.
Imbalance of Enzymes
One possible suggestion of causation is an imbalance of enzymes inside the cornea. Researchers have postulated that this imbalance can cause the cornea to be damaged by free radicals, leading to the characteristic weakness and bulging. This imbalance could explain why the condition seems to be genetic.
Eye Rubbing and Keratoconus
It is unknown exactly how much effect something external such as eye rubbing can have when it comes to this disease. However, there seems to be a correlation with eye rubbing. It cannot be definitively stated that excessive eye rubbing causes keratoconus, but the two things have been linked. It may be that discomfort leading to eye rubbing is actually a symptom rather than a cause. However, most doctors will advise against eye rubbing as it can cause other problems beyond keratoconus. These can include corneal abrasions which can lead to infection or the possibility of transferring germs to the eyes.
Other Causes for Keratoconus
There are other external factors that may cause someone to be more at risk of developing keratoconus. It is thought that damage from ill-fitting contacts or from ultraviolet rays may cause the weakening of the cornea. Any type of injury or irritation to the eye may be connected.
Treatments for Keratoconus
Although the cause may be a little unclear, a surprisingly wide variety of treatments have been discovered to slow or even reverse the effects of keratoconus. These treatments range from non-invasive to moderately invasive and largely depend on the severity of the condition. Here are a few of those treatments.
Contact Lenses for Keratoconus
Although regular lenses do little for the condition, several special types of lenses have been developed to reverse keratoconus. When providing a prescription, the eye doctor takes into account the severity of the condition as well as the priority of the patient. Soft contact lenses are often the most comfortable, but they do not always provide the needed support or the desired sharpness of vision. Gas permeable lenses can provide better vision but are more rigid and therefore less comfortable. Lenses such as scleral contacts and semi-scleral offer greater stability. Different types of contacts can even be combined to provide both functionality and comfort. It is important for the doctor and patient to review all of the options and choose one that best fits the need.
Corneal Crosslinking and Keratoconus
A relatively new treatment for keratoconus is corneal crosslinking. The goal of this procedure is to strengthen the cornea so that it does not become weakened, thin, and bulging. During this procedure, a solution including riboflavin is placed into the eye on the cornea. Ultraviolet light is then carefully placed on the eye. This causes additional bonds to be created in the cornea, strengthening the tissue. If more aggressive treatment is needed, the outside layer of the cornea can be taken off and the treatment can be applied to the deeper areas of the cornea. The outer layer is then replaced after the operation.
Corneal Implants for Keratoconus
In more severe cases, another minimally invasive surgery may be needed to correct the problem. One of these is Intacs corneal inserts. These inserts are made from a see-through dome of polymer that is placed into the cornea. The insert works to change the shape of the cornea to make it less cone-shaped. Intacts have been proven highly effective and have up to a 95% success rate of improving the condition. However, Intacts do not work to strengthen the cornea so in some cases a combination of treatments may be needed.
Corneal Transplant
In extreme cases when no other treatments have been effective, a corneal transplant can be performed on the patient. This may also be necessary in the case of corneal scarring. This surgery is more invasive with longer recovery time. However, the percentage of success for this type of surgery is very high. New breakthroughs have led to procedures that are more accurate, as well as the ability to perform the transplant while leaving the inner layer of the cornea intact. This leads to shorter recovery times as well as less chance of rejection. However, with the option of lenses and crosslinking, the need for corneal transplant for keratoconus patients has dropped to below 5%.
Symptoms of Keratoconus
The symptoms of keratoconus are varied and can be different for each person. Patients first developing the condition may begin to notice some blurriness in their vision due to the improper reception of light into the eye. As it progresses, the patient may notice that certain things in their field of vision begin to look distorted, crooked, or wavy. Many patients have a sensitivity to light and may have a difficult time doing everyday activities such as driving, reading a book, or looking at a computer screen.
After the disease progresses, patients may notice even more blurriness, and may continually need new glasses or contacts because of a rapid increase of nearsightedness or astigmatism. Although the disease does not cause complete blindness, it can cause legal blindness if left untreated, and can seriously inhibit and individual’s ability to lead a normal life. Because it may be difficult to wear contacts in the case of extreme keratoconus, it is best to try to treat the condition early to avoid more invasive procedures. These symptoms can come on gradually, so it is important to have a yearly visit with a Denver eye doctor in order to get an early diagnosis.
Diagnosis Process
A severe case of keratoconus can be immediately apparent during a routine eye exam. Vision problems can be discovered during a basic eye refraction test. During this test, the doctor will check the patient’s vision to see if there are any issues. Many doctors will be able to observe any abnormal curvature using a slit lamp examination. There are also more advanced ways of measuring the curvature of the cornea both to diagnose the disease, and to see if it has progressed. This can be done through a process called topography which creates a map of the cornea for the doctor to read. Any changes in the shape of the cornea will be noted and discussed.
Finding the Right Doctor
It is important to find the right doctor to diagnose and treat keratoconus. The right doctor will be one who will try to correct the problem with the least amount of invasive procedures possible. Depending on whether surgery is needed for the condition, the patient may be working with either an optometrist or an ophthalmologist. These two doctors will often work with the same patient to try to achieve the desired result. In many cases, an optometrist will be able to achieve a satisfactory result from using specialized lenses, and surgery will not be needed.
Frequently Asked Questions
Can You Get LASIK with Keratoconus?
Most eye doctors do not consider patients with keratoconus to be good candidates for LASIK surgery. The reason for this is that during LASIK procedures, small amounts of tissue are taken from the cornea to improve the shape and function of the eye. Because the cornea of the keratoconus patient is already thinned out and weak, this can be unsafe for the patient and cause further problems. Because of these risks, doctors recommend that patients with this disease first work with their optometrist to resolve the keratoconus before beginning to surgically correct additional vision problems.
Is Advanced Keratoconus Considered a Disability?
If left untreated for a long time, keratoconus can cause vision loss that may be severe enough for the patient to be considered legally blind. However, because such successful treatments have been developed for treating this disease, it is rare for it to progress to this stage. If an individual does reach this level of vision loss (usually 20/200 or more severe) even after correction, this person can be considered to be disabled.
Can Keratoconus Lead to Blindness?
Keratoconus does typically progress further over time and becomes worse without treatment. As the disease progresses, vision also degrades. In a typical case, it does not lead to blindness. However, it is important to get treatment because these vision changes can make basic daily tasks difficult and can lead to further problems such as corneal scarring.
What Are the Risk Factors for Keratoconus?
It is possible for anyone to get keratoconus. Studies have shown that ethnicity is not a factor in whether someone is at risk for the disease. However, research has shown that more males get the condition than females. Other risk factors include eye rubbing, badly fitting contact lenses, and eye allergies. As mentioned before, the condition is thought to be genetic, so having someone else in the family with the disease makes it more likely that a person will also develop the disease.
How Can Keratoconus Be Prevented?
If a patient knows that this disease runs in the family, one of the best things that can be done is to prevent the condition from progressing in the first place. One of the best ways to prevent progression is to faithfully have a yearly check-up with the eye doctor. An eye doctor can screen for keratoconus and catch it at its very earliest stages. Treatment for mild keratoconus is much easier.
What Are the Cost Ramifications of Keratoconus Treatment?
Many patients who have been diagnosed with keratoconus may be nervous about how much treatment will cost and whether insurance will cover the treatments and procedures. Of course, the cost will be largely based on how far the disease has progressed and whether surgery is needed. Treatments or surgeries for the condition can cost anywhere from $1,000 to just under $30,000 for a corneal transplant. However, most insurance companies will pay for a majority of these treatments. It is always best for the patient to contact their insurance to find out specifics of the plan.
A diagnosis of keratoconus may be overwhelming at first. Because there is no cure and the condition is progressive, it can be a scary disease to acquire. However, the condition can be effectively treated for years and years. New developments have made it possible to manage keratoconus, reverse its effects, and have great vision without invasive surgeries. Early detection is key, so eye doctors encourage a scheduled yearly visit to keep their patients’ eyes healthy for many years to come.